Today, I pushed myself to go to the funeral home.
I occasionally meet up with a group of wonderful ladies for a walk around the funeral grounds. I used to go a lot, most Mondays in a calendar month but my visits have become non existent. This was my first meet up in awhile.
With the holiday season approaching, many of the ladies expressed their despair. Another holiday without their loved one. Another year coming to an end. Tears flowed. I shared a common bond with one of them---it's hard to watch people grow old while our child remains forever 19. Facebook is becoming a ground of unhappy reminders, time ticking away, friends marrying, grandchildren being born and my child well- she'll never have that.
As I age, my hips are going. I'll need surgery if Jesus is delayed. My mother, 19 years older than I am is hospitalized, her mind dwindling.She is in a convalescent home, far from here. My remaining daughters are working and one is newly married. Is this what they call Empty Nester Syndrome?
We cover: Current Events Suicide Awareness Suicide Prevention World News COVID Mental Health Awareness Mental Illness Anxiety Depression Global Reset Market Crash End Days Currency TRUMP NESARA GESARA Digital Currency Bitt Coin Dinar International News Economics Global Currency Reset Crypto Currency Currencies
Monday, November 30, 2015
Suicide In Canadian Forces
ANDRÉ PICARD
Surgeon-General’s report on suicide in Canadian Forces is cold comfort
The newly released report of the Canadian military’s Surgeon-General on suicide in the Armed Forces makes for chilling reading.
Chilling because of the clinical dispassion with which the numbers are presented.
To wit, here are the key findings, in arduously bureaucratic military language:
- The number of regular-force male suicides was not statistically different than that expected based on Canadian male suicide rates;
- Between 1995 and 2014, there were no statistically significant increases in suicide rates;
- Recent findings suggest a trend towards an elevated suicide rate ratio in regular-force males with a history of deployment;
- Regular-force males under Army command were at significantly increased risk of suicide relative to regular-force males under non-Army commands;
- Regular-force males under Army command in the combat arms trades had statistically significantly higher suicide rates than non-combat arms regular-force males;
- In contrast to previous results, history of deployment may be emerging as a risk factor for suicide in the CAF;
- Results support the theory of a multifactorial causal pathway to suicide rather than a direct link between single risk factors (e.g. PTSD or deployment) and suicide.
Here, by contrast, is what the data say in plain language:
- There is a silent epidemic of male suicide in Canadian society. Things are no better in the military;
- The suicide rate in the Canadian Forces has been high a long time, and it’s getting worse;
- Military personnel who are deployed on overseas missions have a suicide rate that’s 48 per cent higher than those who are not deployed;
- Soldiers in the Army have a suicide rate that is twice the rate of those serving in the Navy and Air Force;
- Soldiers in combat roles have a significantly higher suicide rate than those in non-combat roles – 30 per 100,000 against 18 per 100,000;
- Being deployed on an overseas mission should be considered a risk factor for suicide;
- While deployment and post-traumatic stress disorder are factors, there are a host of reasons military personnel kill themselves.
It
is cold comfort that the suicide rate among males in the Canadian
Forces is the same as among men in the general Canadian population.
In
fact, it’s disturbing. Our soldiers are supposed to be carefully
screened and monitored, in peak condition, physically and mentally.
Presumably, we don’t just send anyone off to war, or on peacekeeping
missions.
But we do know that a significant number come back wounded – and more appear to be wounded mentally than physically.
The
other reason the “it’s no worse in the military than anywhere else”
argument doesn’t hold any water is that, tragically, there’s a silent
epidemic of male suicide.
About 3,000
men take their lives each year in Canada, and there is every indication
that number is an underestimate because a lot of men die “accidental”
deaths in nebulous circumstances. The Surgeon-General’s report, again,
addresses this issue by saying there is no indication suicides by
military personnel are hushed up any more than among civilians.
(We
should note here that the focus is on men because women are not
included in the Canadian Forces report, as they are still a tiny
percentage of military personnel and the suicide numbers are too small
to allow statistical analysis. Men kill themselves at six times the rate
that women do.)
The other blandishment
in the report is the notion that there is “no statistically significant
increase” in suicides. What this means is that, in any given five-year
period, roughly the same number of military personnel kill themselves.
How is that, in any way, a measure of success? It’s actually proof of continued failure.
We are talking about people here – 225 men who have taken their lives between 1995 and 2014.
You can say: That’s not very many, given that there are roughly 57,000 men in the Canadian Forces.
But it is. It’s the equivalent of three giant Hercules aircraft full of combat soldiers crashing and burning.
Defence
Minister Harjit Singh Sajjan is right to demand answers and solutions –
not just superficially soothing statistics – from military brass.
What
he must do next, on this Remembrance Day, is recognize that military
suicide deaths are just as tragic, and just as deserving of recognition
and remembrance, as combat deaths.
That is the surest way of bringing the issue of military suicide out of the shadows.
Are you a member of a military family with a similar story? E-mail Renata D’Aliesio at rdaliesio@globeandmail.com
Parents of British teenager who committed suicide say ‘Wi-Fi allergy’ is to blame in death
A British mother says her daughter committed suicide after suffering an “allergy” to Wi-Fi.
Jennifer Fry was just 15 last spring, when she hanged herself in the woods in Oxfordshire — and her parents Debra Fry and Charles Newman blame wireless signals inside her school.
The parents claim the signals caused Electromagnetic Hypersensitivity Syndrome, with severe headaches, nausea and fatigue as symptoms.
"I intend to carry on my campaign to highlight the dangers of Wi-Fi," she told an Australian news site. "I am not against a bit of technology but I do feel schools should be aware that some children are going to be sensitive to it and reduce its use."
They want Wi-Fi removed from preschools and schools and urge the government to research the syndrome.
Fry admitted she didn’t take Jenny to the doctor, fearful that she would have been institutionalized or given drugs that the mother was suspicious of because the family knew a boy who had committed suicide after being on antidepressants, according to the Mirror, a British publication.
It’s unclear whether “Wi-Fi allergy” exists. Neither the World Health Organization nor the Centers for Disease Control recognize Electromagnetic Hypersensitivity Syndrome as a disease.
 Newsteam/SWNS.com
Newsteam/SWNS.com Jenny Fry, 15, killed herself after developing electro-hypersensitivity from Wi-Fi, according to her parents. She hanged herself in June complaining of exhaustion, headaches and bladder problems that stemmed from the wireless signals at her school.
"The scientific community is still debating: is it real or not real," Sun said. "We should have more investigation and serious consideration for researching this field and we don't know why some people are sensitive to it."
He acknowledges that some people are highly sensitive to magnetic fields, and though previous studies of cell phones found that they were not an inducement for brain tumors, Sun also raised the spectre that no one knows the long-term effects of any of this technology.
"The issue is so hard to prove," Sun said. "People can have a lot of stress and depression. There has to be some evidence to prove it is Wi-Fi induced, otherwise it is very scary. It needs much more research. Maybe that girl was hypersensitive to a magnetic field. It is hard to prove and so far we don't have the scientific data to prove it."
John Harris, a Yale University physics professor, also did not discredit the syndrome, and notes how many of the symptoms are similar to stress. The sensitivity could be to a range of electromagnetic waves.
Some countries are more open to the syndrome as a quantifiable medical issue. France, for example, recently awarded a woman $900 a month in disability because of her ailments with electromagnetic hypersensitivity.
Sunday, November 29, 2015
Reminder / Alert from my Friend
REMINDER...!!!
ALERT...! In case you didn't know...!!There are 3 options that men are receiving and must receive or die during the full reign of the Antichrist.
Once received - your soul is damned.
You have allow Satan sit as God in the temple of God which is your heart if you received it - you received Satan as God the Father, the Beast (given his authority and power) as your savior and messiah (the antichrist), and the false prophet as your evidence of their power (the false prophet - fake rep of holy ghost). This is the trinity of Darkness that sit in the temple of God as God during the great tribulation.
The abomination is upon the temple of God, which you are, and not a
building made with hands, the heart of those who receive the mark of the
beast have become desolate - GOD can never return to His seat in such a
temple - it is destined for everlasting destruction. Hence you cannot
escape everlasting destruction If you received any of them on your skin
or under your skin - they are digital technological applications with
authentication capabilities: Either one of them makes you a member of
the kingdom of the AntiChrist - this technology shall soon be enforced
worldwide as part of the strategy to "Save The World" by combating
"Climate Change" and ensure "Sustainable Development."
1. Mark of the beast - a form of RFID chip
2. Name of the beast - a form of electronic tattoo, also has 666 encoded
3. Number of his name - binary codes.
" He causes all, both small and great, rich and poor, free and slave, to receive a mark on their right hand or on their foreheads, and that no one may buy or sell except one who has THE MARK or THE NAME of the beast, or THE NUMBER of his name.
Here is wisdom. Let him who has understanding calculate the number of the beast, for it is the number of a man: His number is 666. "
Rev 13: 16-18.
WHAT YOU SEE IN THE VIDEO LOOKS LIKE OPTION 2 OR 3.
UN wants to save the planet from "Climate Chaos" - by using "technology for Sustainable Development," UN plan to combat "Climate Change."
Step up for your global ID and become a global citizen! (so that we can track your every move and monitor your carbon footprint, meanwhile the climatic chaos has nothing to do with carbon dioxide).
Have you done your Biometrics? BVN?? Yes... It's a global agenda which shall be used to track every human being so that we can "Save The Planet" and maintain "Sustainable Development."
IT IS THE MARK OF THE BEAST.
1. Mark of the beast - a form of RFID chip
2. Name of the beast - a form of electronic tattoo, also has 666 encoded
3. Number of his name - binary codes.
" He causes all, both small and great, rich and poor, free and slave, to receive a mark on their right hand or on their foreheads, and that no one may buy or sell except one who has THE MARK or THE NAME of the beast, or THE NUMBER of his name.
Here is wisdom. Let him who has understanding calculate the number of the beast, for it is the number of a man: His number is 666. "
Rev 13: 16-18.
WHAT YOU SEE IN THE VIDEO LOOKS LIKE OPTION 2 OR 3.
UN wants to save the planet from "Climate Chaos" - by using "technology for Sustainable Development," UN plan to combat "Climate Change."
Step up for your global ID and become a global citizen! (so that we can track your every move and monitor your carbon footprint, meanwhile the climatic chaos has nothing to do with carbon dioxide).
Have you done your Biometrics? BVN?? Yes... It's a global agenda which shall be used to track every human being so that we can "Save The Planet" and maintain "Sustainable Development."
IT IS THE MARK OF THE BEAST.
Antichrist About to Start WW3 in November??? So Strange!
Another Reminder...! In case you didn't know...!!
There are 3 options that men are receiving and must receive or die during the full reign of the Antichrist.
Once received - your soul is damned.
You have allow Satan sit as God in the temple of God which is your heart if you received it - you received Satan as God the Father, the Beast (given his authority and power) as your savior and messiah (the antichrist), and the false prophet as your evidence of their power (the false prophet - fake rep of holy ghost). This is the trinity of Darkness that sit in the temple of God as God during the great tribulation.
The abomination is upon the temple of God, which you are, and not a building made with hands, the heart of those who receive the mark of the beast have become desolate - GOD can never return to His seat in such a temple - it is destined for everlasting destruction. Hence you cannot escape everlasting destruction If you received any of them on your skin or under your skin - they are digital technological applications with authentication capabilities: Either one of them makes you a member of the kingdom of the AntiChrist - this technology shall soon be enforced worldwide as part of the strategy to "Save The World" by combating "Climate Change" and ensure "Sustainable Development."
1. Mark of the beast - a form of RFID chip
2. Name of the beast - a form of electronic tattoo, also has 666 encoded
3. Number of his name - binary codes.
" He causes all, both small and great, rich and poor, free and slave, to receive a mark on their right hand or on their foreheads, and that no one may buy or sell except one who has THE MARK or THE NAME of the beast, or THE NUMBER of his name.
Here is wisdom. Let him who has understanding calculate the number of the beast, for it is the number of a man: His number is 666. "
Rev 13: 16-18.
UN wants to save the planet from "Climate Chaos" - by using "technology for Sustainable Development," UN plan to combat "Climate Change."
Step up for your global ID and become a global citizen! (so that we can track your every move and monitor your carbon footprint, meanwhile the climatic chaos has nothing to do with carbon dioxide).
Have you done your Biometrics? BVN?? Yes... It's a global agenda which shall be used to track every human being so that we can "Save The Planet" and maintain "Sustainable Development."
IT IS THE MARK OF THE BEAST.
Saturday, November 28, 2015
Her Latest Concert Miley Cyrus WARNING:Graphic
 I have told my daughters that the Kardashians, are witches, engage in human sacrifice, and so does Madonna, and Miley, and Madonna and others. The latest Kardashian nail styles are pointy, just like animal claws, that came to my attention. We must be informed and diligent in protecting the minds of our youth.. This is not just a sexual propoganda, but a spiritual war on the minds of our youth. If you go into Amazon, and look at the lyrics of the songs they sing, you will be more appalled at the words than these pictures..Must pass on as the minds of our your are destroyed.. for lack of knowledge.
I have told my daughters that the Kardashians, are witches, engage in human sacrifice, and so does Madonna, and Miley, and Madonna and others. The latest Kardashian nail styles are pointy, just like animal claws, that came to my attention. We must be informed and diligent in protecting the minds of our youth.. This is not just a sexual propoganda, but a spiritual war on the minds of our youth. If you go into Amazon, and look at the lyrics of the songs they sing, you will be more appalled at the words than these pictures..Must pass on as the minds of our your are destroyed.. for lack of knowledge.
Climate Summit-Not About Carbon
News Feed
OK,A friend has encouraged me to post this, I believe I should. I understood this some time last month, but now I shall post a summary, if my understanding is correct, then... We Are Here at A Time In History!
United Nations (UN) Framework Convention on Climate Change:
Paris Climate Change Conference holds from 30th November to 11th December 2015. At least 147 heads of state shall attend. All the leaders of this world shall sit down for 2 weeks to discuss Climate Change.
Do you remember the 500 days to avoid Climatic Chaos by the French Foreign Minister? That was pointing to the 70th UN General Assembly which held in September 2015, where the agenda for a New World Order (NWO) via the UN was endorsed by all world leaders. All the nations of the world signed off their sovereignty to the UN under the Agenda 21 or Post 2015 Agenda or Agenda 2030 (whatever they call it) which is designed to "save the Planet" by ensuring "Sustainable Development." They are expecting a Climatic Chaos, but they deceive us by telling us that it is caused by Carbon emissions. This Agenda and the 70th UN General Assembly also resulted to this Paris Climate Change Conference.
The only ingredient to fully enforce this NWO Agenda to every human being in this world is a Climatic Chaos. Again, they are expecting a Climatic Chaos, that is why world leaders can agree to meet for 2 weeks to "discuss Carbon emissions," do not be deceived - the Climatic Chaos has nothing to do with Carbon emissions.
This UN Climate Convention in Paris is very important to impose the NWO. During the Convention, I expect something serious to happen, yes, the Climatic Chaos they expect is likely to begin before the end of the Convention in Paris, so that when the world is terrified by the Climatic Chaos, all people shall accept whatever the leaders at the UN Convention impose on them, and all men shall accept the NWO Agenda to "Save the Planet," including the mark of the beast, one world religion, and all the details in Agenda 21.
A leader shall possibly be selected to lead this UN move to save the Planet from Climatic Chaos: this leader shall likely be the Anti-Christ.
So, if it is not Carbon emissions that shall bring about this Climatic Chaos, what shall it be...?!
Planet-X or Nibiru.
The sightings are numerous, to deny that it's out there is foolish foolishness; even ordinary people have seen it and taken videos and pictures - especially over the last few months. VERY SOON ALL MEN SHALL SEE PLANET-X IN THE SKY, AND THEY SHALL MOURN.
Planet X, a huge planetary body, or star, that entered our Solar system and is headed our way. Described as a great “Red Star,” the path of this approaching, heavenly object puts it on a potential, near collision course with our planet earth. But even if it does not collide with the earth, it shall come close enough to cause catastrophic damage.
"There is a very large debris field around the planet x system. We will see the stars as though they are falling from the sky and the sky will look as if it is rolling up like a scroll when it passes us and heads back out to space." Patti Benner
They have seen it for years, they have been expecting it, they have prepared underground shelters, they have made preparations for the death of a large percentage of the earth's population, they have stored all the seeds that they can find, they have made preparations for a post-normal world. The potential destruction of the earth by this catastrophe is expected. When the cataclysmic events begin - the world leaders shall already be gathered together - they shall go into their safe caves and holes and shelters underground - along with many Elites who have prepared, and many others who are selected. They cannot make provision for the whole population - therefore the rest of mankind shall ride out the Climatic Chaos.
Many other things shall also begin to happen: nations shall rise up against nations, there shall be betrayals, deaths, treason, too much to say.
Bride of Christ, rejoice...!
When the days of darkness begins, and the heavens and the earth are shaken, then shall our redemption be sure. We can be sure that the LORD shall protect all of His during the Climatic beginning of the Cataclysmic Event, until the day He takes us out of the earth - before the main event. But surely - the Bride of Christ shall witness a Cataclysmic event on the earth before they are taken out. Congratulations, be Rapture ready.
For the rest of mankind that are not preserved in Christ Jesus, and for the Lukewarm Christians, shall be... the worst days of the Great Tribulation which they shall weep and wail and die and cry, but it shall be too late: there shall be no more love, no more grace, no more peace on the earth.
Again, the UN Climate Convention in Paris is from 30th November to 11th December 2015: you might want to read through this note again.
REPENT AND BE CONVERTED TO CHRIST!
THE KING IS COMING!!
JESUS IS COMING.
" The loftiness of man shall be bowed down, And the haughtiness of men shall be brought low; The Lord alone will be exalted in that day, ... They shall go into the holes of the rocks, And into the caves of the earth, From the terror of the Lord And the glory of His majesty, When He arises to shake the earth mightily. " Isaiah 2:17-19.
"Immediately after the tribulation of those days the sun will be darkened, and the moon will not give its light; the stars will fall from heaven, and the powers of the heavens will be shaken. THEN THE SIGN OF THE SON OF MAN WILL APPEAR IN HEAVEN, and then ALL THE TRIBES OF THE EARTH WILL MOURN, and they will see the Son of Man coming on the clouds of heaven with power and great glory. And He will send His angels with a great sound of a trumpet, and they will gather together His elect from the four winds, from one end of heaven to the other."
Matt 24:29-31.
"And there will be signs in the sun, in the moon, and in the stars; and on the earth distress of nations, with perplexity, the sea and the waves roaring; men's hearts failing them from fear and the expectation of those things which are coming on the earth, for the powers of the heavens will be shaken.
Then they will see the Son of Man coming in a cloud with power and great glory. Now when these things begin to happen, look up and lift up your heads, because your redemption draws near."
"...But take heed to yourselves, lest your hearts be weighed down with carousing, drunkenness, and cares of this life, and that Day come on you unexpectedly. For it will come as a snare on all those who dwell on the face of the whole earth. Watch therefore, and pray always that you may be counted worthy to escape all these things that will come to pass, and to stand before the Son of Man."
Luke 21:25-36.
" I looked when He opened the sixth seal, and behold, there was A GREAT EARTHQUAKE; and the SUN BECAME BLACK as sackcloth of hair, and the MOON BECAME LIKE BLOOD. And the STARS OF HEAVEN FELL TO THE EARTH, as a fig tree drops its late figs when it is shaken by a mighty wind. Then the sky receded as a scroll when it is rolled up, and every mountain and island was moved out of its place. And the kings of the earth, the great men, the rich men, the commanders, the mighty men, every slave and every free man, HID THEMSELVES IN THE CAVES AND IN THE ROCKS OF THE MOUNTAINS, and said to the mountains and rocks, "Fall on us and hide us from the face of Him who sits on the throne and from the wrath of the Lamb! For the great day of His wrath has come, and who is able to stand?"
"AFTER THESE THINGS I saw four angels standing at the four corners of the earth, holding the four winds of the earth, that the wind should not blow on the earth, on the sea, or on any tree. Then I saw another angel ascending from the east, having the seal of the living God. And he cried with a loud voice to the four angels to whom it was granted to harm the earth and the sea, saying,"Do not harm the earth, the sea, or the trees till we have sealed the servants of our God on their foreheads." And I heard the number of those who were sealed. One hundred and forty-four thousand of all the tribes of the children of Israel were sealed:"
" AFTER THESE THINGS I looked, and behold, a great multitude which no one could number, of all nations, tribes, peoples, and tongues, standing before the throne and before the Lamb, clothed with white robes, with palm branches in their hands, and crying out with a loud voice, saying,"Salvation belongs to our God who sits on the throne, and to the Lamb!" All the angels stood around the throne and the elders and the four living creatures, and fell on their faces before the throne and worshiped God, saying: "Amen! Blessing and glory and wisdom, Thanksgiving and honor and power and might, Be to our God forever and ever. Amen." Then one of the elders answered, saying to me,
"WHO ARE THESE ARRAYED IN WHITE ROBES, and WHERE did they come from?"
And I said to him, "Sir, you know." So he said to me,
"THESE ARE THE ONES WHO COME OUT OF THE GREAT TRIBULATION, and WASHED THEIR ROBES AND MADE THEM WHITE IN THE BLOOD OF THE LAMB.”
“Therefore they are before the throne of God, and serve Him day and night in His temple. And He who sits on the throne will dwell among them. They shall neither hunger anymore nor thirst anymore; the sun shall not strike them, nor any heat; for the Lamb who is in the midst of the throne will shepherd them and lead them to living fountains of waters. And God will wipe away every tear from their eyes."
Rev 6:12-17, Rev 7:1-4, 9-17.
Friday, November 27, 2015
Movember Foundation-Men's Mental Health
Douglas Todd: Unprecedented effort to improve men’s mental health
Known for its fight against men’s cancers, the Movember Foundation’s foray into men’s mental health has already outspent government on research
By Douglas Todd, Vancouver Sun Columnist
August 21, 2014

UBC Prof. John Ogrodniczuk (left) and Prof. John Oliffe have received $2.9 million in funding to support men’s mental health, such as suicide prevention and anti-depression programs.
Photograph by: Kim Stallknecht , PNG
Two months
before comedian Robin Williams ended his life, a photo exhibit called
Man-Up Against Suicide was drawing in audiences at the Foster Eastman
art gallery in downtown Vancouver.
The riveting exhibition featured the photographs of 25 men and women who have been shaken by male suicide. The display was funded by the Movember Foundation, the international men’s health initiative best known for its November moustaches campaign.
But the Man-Up Against Suicide exhibit, which will soon go on tour, is just a small part of Movember’s unprecedented $12-million Canadian campaign to strengthen men’s mental health, particularly in regard to male suicide and depression.
Last year, for the first time in Canada, the Movember Foundation — founded 11 years ago in Australia and now in 21 countries — began to add men’s mental health to its focus on prostate and testicular cancer.
As a result, new Movember Foundation grants immediately surpassed the total amount of money all levels of governments across Canada have devoted to targeted mental health programs for men.
Two University of B.C. professors — John Oliffe from nursing and John Ogrodniczuk from psychiatry — are co-leaders of a project funded by a Movember grant of $2.9 million (including the photo exhibit).
The professors cite chilling statistics: The suicide rate for men and boys is four times higher than it is for girls and women. Yet few Canadians talk specifically about men’s mental health.
Among other things, Ogrodniczuk and Oliffe are trying to overcome men’s reluctance to deal with mental health difficulties.
Recognizing that about 70 per cent of Canadians who seek mental health treatment are women, the two specialists are trying to break down barriers that keep many men from seeking support.
Some ideals of masculinity, based on “emotional stoicism” and not expressing sadness, can get in the way. But they say professionals can still connect with men’s yearning for healthy lives by appealing to other masculine values, such as working hard, taking action and showing courage.
To such ends, the professors are overseeing five projects devoted to raising awareness and directly supporting men in B.C. and beyond, including seniors, soldiers, post-secondary students and aboriginals.
“The $12 million that Movember Canada is spending on men’s mental health is unprecedented,” said Oliffe, explaining that it dwarfs what Canada’s government-funded health research bodies have spent in the field in the past 15 years.
“I’ve never seen this kind of support before. And it’s going to make a difference.”
The Aug. 11 suicide of Williams led more people to engage in “powerful” talk about male depression, said Oliffe. People are recognizing that even globally celebrated men can live in severe isolation, and don’t reach out for help.
One of the UBC team’s plans is to design a state-of-the-art website for men falling into suicidal thoughts and depression (which is often not recognized in men).
Researchers have discovered depression is as prevalent among men as women. However, its symptoms are different in men, and include irritability, risky behaviour and escape mechanisms such as workaholism and alcohol abuse. The website will attempt to overcome stereotypes about men and mental health.
For instance, one study Ogrodniczuk took part in found men referred to Richmond Hospital’s mental health program were just as ready as women to enter into psychotherapy.
Another one of UBC’s Movember projects centres on men with recent diagnoses of prostate cancer, because they are at higher risk for depression. An other is for young men struggling with the tough transition to college or university, where they often experience loneliness and overwhelming pressure to succeed.
These male transition programs are led by Marv Westwood of UBC’s counselling psychology department, who bases his approach on groups he has operated for soldiers re-entering civilian life.
Another Movember pilot project in B.C. is called The Dude’s Club, led by Dr. Paul Gross. It aims to give emotional support to First Nations men in Vancouver’s Downtown Eastside.
Men’s Sheds in Kelowna and Winnipeg, give older men a chance to “come together in the way guys do,” says Ogrodniczuk, whose rural Alberta upbringing and amateur hockey career has given him first-hand experience with “tough” males.
Meanwhile, the Man-Up Against Suicide exhibition is to go on display on Sept. 10 (World Suicide Prevention Day) at Valley View Funeral Home in Surrey, as well as next month in the small Alberta town of Rimbey (in part because men’s suicide rates are higher in rural areas).
Across Canada, in addition to funding prostate and testicular cancer programs, Movember is sponsoring other creative efforts to bolster men’s mental health.
They include a $3-million grant to overcome Canadian Asian males’ stigma against mental illness; a $480,000 project to support “healthy dads,” and a $1.7-million plan to reduce the misuse of drugs and alcohol among male post-secondary students.
One of the professional skills necessary to assist males in dealing with often-ignored mental health issues, say Ogrodniczuk and Oliffe, requires approaching them with the right pitch — because many men, unlike women, are often put off by language that typically surrounds therapy, seeking help and sharing feelings.
Ogrodniczuk talks about the importance of mental-health professionals using alternative language with men — including offering to consult with them, as opposed to provide therapy, and to not be shy about swearing in support sessions, since many men find it natural.
As for suicidal thoughts, Oliffe witnessed many men trying to deny their pain when he worked in Australian emergency departments. He emphasizes building hope on the masculine values of not letting others down — and continuing to be a strong provider for family.
The Movember grant to the UBC team expires at the end of 2016, but the professors are working to find ways to extend their men’s mental health projects beyond that date. A lot of people, men and women, are counting on them.
dtodd@vancouversun.com
Blog: www.vancouversun.com/the search
The riveting exhibition featured the photographs of 25 men and women who have been shaken by male suicide. The display was funded by the Movember Foundation, the international men’s health initiative best known for its November moustaches campaign.
But the Man-Up Against Suicide exhibit, which will soon go on tour, is just a small part of Movember’s unprecedented $12-million Canadian campaign to strengthen men’s mental health, particularly in regard to male suicide and depression.
Last year, for the first time in Canada, the Movember Foundation — founded 11 years ago in Australia and now in 21 countries — began to add men’s mental health to its focus on prostate and testicular cancer.
As a result, new Movember Foundation grants immediately surpassed the total amount of money all levels of governments across Canada have devoted to targeted mental health programs for men.
Two University of B.C. professors — John Oliffe from nursing and John Ogrodniczuk from psychiatry — are co-leaders of a project funded by a Movember grant of $2.9 million (including the photo exhibit).
The professors cite chilling statistics: The suicide rate for men and boys is four times higher than it is for girls and women. Yet few Canadians talk specifically about men’s mental health.
Among other things, Ogrodniczuk and Oliffe are trying to overcome men’s reluctance to deal with mental health difficulties.
Recognizing that about 70 per cent of Canadians who seek mental health treatment are women, the two specialists are trying to break down barriers that keep many men from seeking support.
Some ideals of masculinity, based on “emotional stoicism” and not expressing sadness, can get in the way. But they say professionals can still connect with men’s yearning for healthy lives by appealing to other masculine values, such as working hard, taking action and showing courage.
To such ends, the professors are overseeing five projects devoted to raising awareness and directly supporting men in B.C. and beyond, including seniors, soldiers, post-secondary students and aboriginals.
“The $12 million that Movember Canada is spending on men’s mental health is unprecedented,” said Oliffe, explaining that it dwarfs what Canada’s government-funded health research bodies have spent in the field in the past 15 years.
“I’ve never seen this kind of support before. And it’s going to make a difference.”
The Aug. 11 suicide of Williams led more people to engage in “powerful” talk about male depression, said Oliffe. People are recognizing that even globally celebrated men can live in severe isolation, and don’t reach out for help.
One of the UBC team’s plans is to design a state-of-the-art website for men falling into suicidal thoughts and depression (which is often not recognized in men).
Researchers have discovered depression is as prevalent among men as women. However, its symptoms are different in men, and include irritability, risky behaviour and escape mechanisms such as workaholism and alcohol abuse. The website will attempt to overcome stereotypes about men and mental health.
For instance, one study Ogrodniczuk took part in found men referred to Richmond Hospital’s mental health program were just as ready as women to enter into psychotherapy.
Another one of UBC’s Movember projects centres on men with recent diagnoses of prostate cancer, because they are at higher risk for depression. An other is for young men struggling with the tough transition to college or university, where they often experience loneliness and overwhelming pressure to succeed.
These male transition programs are led by Marv Westwood of UBC’s counselling psychology department, who bases his approach on groups he has operated for soldiers re-entering civilian life.
Another Movember pilot project in B.C. is called The Dude’s Club, led by Dr. Paul Gross. It aims to give emotional support to First Nations men in Vancouver’s Downtown Eastside.
Men’s Sheds in Kelowna and Winnipeg, give older men a chance to “come together in the way guys do,” says Ogrodniczuk, whose rural Alberta upbringing and amateur hockey career has given him first-hand experience with “tough” males.
Meanwhile, the Man-Up Against Suicide exhibition is to go on display on Sept. 10 (World Suicide Prevention Day) at Valley View Funeral Home in Surrey, as well as next month in the small Alberta town of Rimbey (in part because men’s suicide rates are higher in rural areas).
Across Canada, in addition to funding prostate and testicular cancer programs, Movember is sponsoring other creative efforts to bolster men’s mental health.
They include a $3-million grant to overcome Canadian Asian males’ stigma against mental illness; a $480,000 project to support “healthy dads,” and a $1.7-million plan to reduce the misuse of drugs and alcohol among male post-secondary students.
One of the professional skills necessary to assist males in dealing with often-ignored mental health issues, say Ogrodniczuk and Oliffe, requires approaching them with the right pitch — because many men, unlike women, are often put off by language that typically surrounds therapy, seeking help and sharing feelings.
Ogrodniczuk talks about the importance of mental-health professionals using alternative language with men — including offering to consult with them, as opposed to provide therapy, and to not be shy about swearing in support sessions, since many men find it natural.
As for suicidal thoughts, Oliffe witnessed many men trying to deny their pain when he worked in Australian emergency departments. He emphasizes building hope on the masculine values of not letting others down — and continuing to be a strong provider for family.
The Movember grant to the UBC team expires at the end of 2016, but the professors are working to find ways to extend their men’s mental health projects beyond that date. A lot of people, men and women, are counting on them.
dtodd@vancouversun.com
Blog: www.vancouversun.com/the search
© Copyright (c) The Vancouver Sun
Deborah's Friend

Sweet , Sweet girl from elementary school.. Thanks darlin, for who you are.. Love you, and Jesus loves you.
The Trap of Luke 21;35 Is Now Set
Fwd: THE TRAP OF LUKE 21:35 IS NOW SET, AND READY TO BE SPRUNG!
From: Rgreese49@aol.com
To: rgreese49@aol.com
Sent: 11/25/2015 10:18:43 P.M. Eastern Standard Time
Subj: THE TRAP OF LUKE 21:35 IS NOW SET, AND READY TO BE SPRUNG!
THE TRAP OF LUKE 21:35 IS SET AND READY TO BE SPRUNG!In Luke 21:34--36, Jesus says, "...so THAT DAY come upon you unawares (unexpectedly). For as a SNARE (OR TRAP) shall it come on all them, who dwell on the face of the whole earth. Watch ye therefore, and pray always, that ye may be accounted worthy, to ESCAPE ALL THESE THINGS , and to stand before the Son of man (Jesus)."Please notice the words "THAT DAY" and "ESCAPE ALL THESE THINGS". These verses are obviously referring to THE DAY OF OUR ESCAPE, THE RAPTURE. If you read these verses carefully, Jesus is telling us, once again, that THE DAY OF THE RAPTURE AND THE DAY OF THE SNARE, OR TRAP (THE SUDDEN DESTRUCTION of 1st Thess. 5:3), ARE AT THE VERY SAME TIME.So, if we want to know the DAY OF THE RAPTURE, WE SHOULD BE LOOKING FOR THE DAY OF THE TRAP. What is this trap that Jesus is referring to, and who is setting this trap? Is Jesus, or God, setting a trap for us? Not the God, and Jesus, whom I serve. It is Satan who has been setting this trap for the end-times for decades, and probably centuries.Yes, Satan is in the Final stages of his evil, diabolical, and sinister plan to control this world. His instrument is the extremely arrogant and evil New World Order elite. Yes, you must believe they have a plan. This plan has now come to its VERY LAST STEP. They have already set the TRAP and IT IS NOW READY TO BE SPRUNG, in the form of their Planned Sudden Destruction, which will start World War 3. As these verses tell us, it is a TRAP THAT IS COMING UPON THE WHOLE WORLD.It is a deadly trap. It is an evil, diabolical snare, to encompass the entire world. Their Satanic goal is a one-world government, with a one-world dictator, a one-world religion, a one-world economic system (referred to as the Mark of the Beast), and a one-world legal system (which I believe will be Muslim sharia law--what other legal system chops off the heads of non-believers?)Before we discuss how this snare, or trap, is about to be sprung on the whole world, let's discuss what the setting of the trap was. Yes, "WAS". The trap has already been set. It is now history. This trap will NOT be unset. It is too late for that. The springing of this trap, the Final step to Satan's plan for ultimate control, is now literally at our doorstep, and is, almost certainly, only days, or weeks, away from being sprung.So, what is the trap that has already been set, and cannot be reversed? What has the NWO elite done that would qualify as the "Setting of the snare, or trap, of Luke 21:35"? They have been working on this evil, sinister plan for decades. All of the pieces on the chessboard are in place, except for one piece. Any day now, the New World Order elite will announce to the entire world, "CHECKMATE". The trap will have been sprung, the moment they move that last piece on the chessboard.
They have been giving us all of the signs that everything now is in place, ready for their very last move. Their last move, using chess analogy, will be to take out the Queen, and trap the King, all in one well-orchestrated move. Game over. Trap sprung. Too late now. No more signs. Millions (perhaps hundreds of millions) die at the time of the Snare, or Trap, which is the Sudden Destruction, which likely begins the Tribulation hour. Now that we sit at the very brink of World War 3, the party is over for the world, and for all of those Christians who were not ready.The goal of the New World Order elite is a one-world government, with a one-world leader, or President, or Dictator, in control. Their goal includes a new-age Messiah, someone who can control the masses of people, through their allegiance to him. He will have to be a Christ-like figure, extremely popular around the world. During the first half of the Final 7 Years, he will be extremely deceptive, yet a man of peace, such as a Nobel Peace Prize winner, who will be setting the stage for the springing of the trap of the NWO elite. Even the majority of Christians will not be able to recognize him, for who he really is. It is a time of MASS DECEPTION, LED BY THE GREAT DECEIVER.The last move on the chessboard will involve the demise, or destruction, of the United States. When they announce "CHECKMATE", the United States, the Queen nation, protecting the King nation of Israel, will no longer be a world power. This is their last move on the chessboard. All other pieces are now in place. The demise of the U.S. is the FINAL chess move on their diabolical agenda. It is the Game Changer. THE DEMISE OF THE UNITED STATES IS THE SPRINGING OF THE TRAP.But what was the SETTING of the trap? We, the people of the United States, set our own trap!!! If the NWO elite could just get THEIR CHOSEN MAN, THEIR NEW-AGE MESSIAH, THEIR CHARISMATIC LEADER, THE GREAT DECEIVER, INTO POWER, AS PRESIDENT OF THE U.S., THE FINAL TRAP WOULD BE SET!!! So, they planted their CHOSEN MAN, BARACK HUSSEIN OBAMA, in this country, and destined him to become the President of the one nation, which was standing in their way of a one-world government.With the generous help of the sheeple of the U.S., we fell right into their trap. I did not vote for this Great Deceiver, but many of you reading this post, did vote for him. You have helped set the GREATEST SATANIC TRAP IN ALL OF HUMAN HISTORY, by elected the Antichrist to be the President of the United States. Repent, and the Lord will forgive you. But now, there is NO turning back. Their man of Great Deception is now in power.Yes, our once-great country has set our own irreversible trap. On Oct. 29, 2008, Obama made his covenant with millions upon millions of people to RADICALLY CHANGE THE UNITED STATES, AND TO CHANGE THE WORLD!!! As a nation, we returned the favor to him, and to the New World Order elite, one week later, by electing the Beast of Revelation, as our President. As a result of this "Setting of the Trap", we have pronounced judgment on ourselves. The Satanic NWO will be the instrument used to carry out this judgment. With less than one year left as President of the U.S., the NWO is quickly running out of time, to spring this MASSIVE TRAP OF UNPARALLELED DECEPTION, AND UNBELIEVABLE HORROR!It is my firm conviction that our country is about to be betrayed by the Great Deceiver, the Biblical Antichrist, the trap-setting agent, Barack Hussein Obama. He has been planted here by the NWO elite. That is why all of his records are hidden. That is why there is so very little that we really know about this mystery man. His birth certificate, his college records, his childhood, his social security number, no history of any girl friends, and the list goes on and on and on, about this mystery man. He escapes scrutiny, with the help of Satan, and because of the widespread and total control of the media, by the NWO elite. He seems untouchable.The Lord is allowing Satan to execute this evil, sinister, and diabolical plan, but only for a short time. Satan knows that his time is short, but it is not stopping him from pulling out all of the stops, in his last-ditch effort to control this world.Yes, in my opinion, THE PLANTING, BY THE NWO, OF BARACK HUSSEIN OBAMA, AS PRESIDENT OF THE U.S., WAS THE SETTING OF THE TRAP OF LUKE 21:35. The demise of the U.S., which is the Springing of the Trap, will greatly affect the entire world. Israel, the King nation, will no longer have the U.S., the Queen nation, to protect her. World War 3 will erupt, with the unleashing of the GREAT SWORD (nuclear weapons?) in Rev. 6. Out of the ashes and chaos of World War 3, the New World Order will emerge. This is the motto of the New World Order.How will the NWO elite Spring the Trap that has been already Set? We can only speculate. I believe that Obama hates the United States, and is an integral part of the destruction, or demise, of our country. He has proven that in the past SEVEN years. If this is true, then he will have no hesitation in NOT retaliating, when the bombs are in the air from another country, or perhaps planted here by the NWO elite, with ISIS having now been set up as the scapegoat. He will be underground, or out of the country.
Is it part of the NWO's well-orchestrated plan to have Obama, Putin, and all of the world leaders, together in Paris, France, during the time of Nov. 30th through Dec. 11th, so that Obama will be thousands of miles from the destruction of the U.S.??? The first week of December, 2015, is an extremely high RAPTURE ALERT TIME!!! To put this evil, scheming, deceptive traitor, as the one with his finger on the retaliatory nuclear button, IS THE ULTIMATE GREAT TRAP, that we have set for ourselves.Certainly, we should not expect the Antichrist to attempt to SAVE our country. He was planted here to DESTROY our country. It is the downfall, or demise, of the United States, that will cause Obama to be the King of the World, as this will force a one-world government to quickly come to the forefront. What form of TRAP, OR SNARE, does the NWO have in mind? The Word does not make it clear. Perhaps a limited nuclear war. Perhaps an EMP attack, with just one nuclear missile launched off the West Coast, exploding miles above the ground, which would totally destroy the entire electrical grid of the United States, setting our country into the Dark Ages, for the entire length of the Tribulation.Or, perhaps a Planned Sudden Destruction, of a man-made (HAARP) mega-earthquake on the West Coast, with a resulting catastrophic tsunami, killing millions of people. Or, maybe the same thing on the New Madrid fault line, where many of our country's nuclear power plants lie. Whatever this TRAP,or SNARE, of Luke 21 is, it will be MASSIVE AND EXTREMELY CATASTROPHIC. It HAS to be, to bring about the one-world government. The United States, because of its power, is standing in the way of the diabolical, evil, scheming New World Order elite, and the formation of their one-world government.In my opinion, THE TIMING OF THE SPRINGING OF THIS TRAP, THAT HAS ALREADY BEEN SET, IS LIKELY TO BE DECEMBER, 2015, ESPECIALLY THE FIRST WEEK!!!
The man whom the world looks upon as the
Nobel
Peace
prizewinner is about to become the one who
takes peace
from the earth. We can only
speculate as to the
countries involved. But, based
on the content of
this post, Obama will betray our
country, and then
fail to retaliate, by not pushing the nuclear
button.
Perhaps the perfect
excuse will be because he has
just suffered the
mortal head wound in Revelation 13,
and is unable to
respond. Perhaps part
of this SNARE,
or TRAP, is that
Obama will have
just suffered an
"assassination" attempt on
his life. Perhaps the False
Prophet (Pope
Francis?) will be there, in Paris, France, to
attempt to
resurrect Obama back to life.
But before that
could possibly happen, will the deadly Planned
Sudden
Destruction, or demise, of
the United States have taken
place? One
has to wonder, even as I write this, if all
the final details
of this, or a similar, plan are in the Final
stages of
preparation.
The counterattack by Jesus, of Satan's extremely evil scheme, will be the Rapture of the Bride. Hallelujah!!! Luke 21:34--36, which promises this SNARE, OR TRAP, TO COME UPON THE WHOLE WORLD, ALSO PROMISES A GREAT ESCAPE FROM ALL THESE THINGS. THAT GREAT ESCAPE IS THE RAPTURE OF THE BRIDE!!!Jesus would say unto us this very day, "Be holy, for without holiness, no man will see the Lord. Separate yourselves from the world, and THEN I will receive you unto Myself. Do NOT lose your first love. Do NOT become lackadaisical in your spiritual walk. Repent of all sin in your life. Turn completely away from sin, and turn unto me. I will give you power over sin, if you will yield to me. I wish that you were either hot or cold, but because you are lukewarm, I MUST spue some of you out of my mouth."
"Many of
you must make your soiled garments white again, in the Hour of testing that is
coming upon the whole world. My children, prepare to meet your
God. Make spiritual preparation, to become part of my
Bride. My Bride makes herself ready. The Day will SOON be upon
you. I want you to be part of my pure and spotless
Bride. Prepare, my children. The hour is VERY VERY
VERY late."
Maranatha!Ron Reese
|  | |||
| ||||
Thursday, November 26, 2015
US Approval caused the Russian Jet to be Shot Down
Turkey can’t shoot down Russian jet without US approval: Analyst
Fri Nov 27, 2015
http://www.presstv.com/Default/Section/130
http://www.bbc.com/news/world-middle-east-34913010

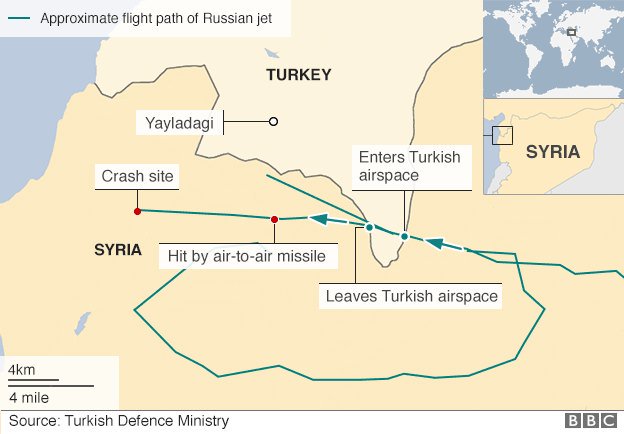
PressTv User
Turkey cannot take a
dangerous action like the shooting down of a Russian warplane without
getting the approval from the United States, says Myles Hoenig, an
American political analyst and activist in Maryland.
Russian President Vladimir Putin announced on Thursday that Moscow had provided prior information to Washington of the flight path of the aircraft shot down by Ankara inside Syria near the Turkish border this week.
"The American side, which leads the coalition that Turkey belongs to, knew about the location and time of our planes' flights, and we were hit exactly there and at that time," Putin said at a joint press conference with French President Francois Hollande in Moscow.
Commenting to Press TV, Hoenig said, “If the charges by Putin are true, it’s a clear sign that the affects of US foreign and military policy is to further de-stabilize an already chaotic and distressed part of the world.”
“One can only wonder how this insanity of goading Russia into a fight with NATO has taken full control of the Obama White House,” he added.
On Tuesday, NATO member Turkey shot down a Russian Sukhoi Su-24 Fencer jet, claiming the aircraft had repeatedly violated its air space.
Putin said the jet had been attacked when it was 1 kilometer inside Syria. He warned of "serious consequences" and called it a “stab in the back” administered by "the accomplices of terrorists."
Russia has been conducting airstrikes on Daesh (ISIL) positions at the request of the Syrian government since September 30.
Jet downing shows US 'desperation'
“Russia has pretty much stepped in where the Western powers have shown either an unwillingness or inability to end the ISIS terror,” Hoenig said, using an alternative acronym for the terrorist organization.
“This is changing the balance of power in the Middle East and the US is losing standing worldwide due to this. Yet allowing for an attack on a Russian military plane shows desperation on the part of the US and its allies. It is incredibly dangerous as the two military powers could easily destroy each other and all others on the planet,” he noted.
“US policy in the Middle East has no clear vision. It claims it wants an end to ISIS yet seems to be dancing around when it comes to going after them. Are they waging a war against ISIS? Or, are they funding and supplying them? Or is the US goal foremost to take out the Assad government, with any damage to the ISIS powers being secondary?” the analyst wondered.
“It is not hard to believe that all that Turkey has been doing has been with full knowledge of its US controllers. Its primary goals are to see an end to the Assad regime (similar to that of the US) but also to prevent any kind of Kurdish independence,” he stated.
“Turkey knows that what it does militarily will be supported by NATO so all such actions must have US approval which would draw the Russian military into a combat situation with the US or its allies,” Hoenig concluded.
US 'concerned' over S-400 deployment
The Kremlin has announced that it is sending S-400 anti-aircraft missiles to Latakia in northwestern Syria in the wake of the shooting down the Russian warplane.
The US military is very concerned about Russia’s imminent deployment of the advanced missile defense system to Syria, according to an American official.
The official, speaking on condition of anonymity, said on Wednesday the S-400 poses a significant threat. He said the planned deployment is raising “significant concerns” for the US military, which is conducting airstrikes in Syria.
Russian President Vladimir Putin announced on Thursday that Moscow had provided prior information to Washington of the flight path of the aircraft shot down by Ankara inside Syria near the Turkish border this week.
"The American side, which leads the coalition that Turkey belongs to, knew about the location and time of our planes' flights, and we were hit exactly there and at that time," Putin said at a joint press conference with French President Francois Hollande in Moscow.
Commenting to Press TV, Hoenig said, “If the charges by Putin are true, it’s a clear sign that the affects of US foreign and military policy is to further de-stabilize an already chaotic and distressed part of the world.”
“One can only wonder how this insanity of goading Russia into a fight with NATO has taken full control of the Obama White House,” he added.
On Tuesday, NATO member Turkey shot down a Russian Sukhoi Su-24 Fencer jet, claiming the aircraft had repeatedly violated its air space.
Putin said the jet had been attacked when it was 1 kilometer inside Syria. He warned of "serious consequences" and called it a “stab in the back” administered by "the accomplices of terrorists."
Russia has been conducting airstrikes on Daesh (ISIL) positions at the request of the Syrian government since September 30.
Jet downing shows US 'desperation'
“Russia has pretty much stepped in where the Western powers have shown either an unwillingness or inability to end the ISIS terror,” Hoenig said, using an alternative acronym for the terrorist organization.
“This is changing the balance of power in the Middle East and the US is losing standing worldwide due to this. Yet allowing for an attack on a Russian military plane shows desperation on the part of the US and its allies. It is incredibly dangerous as the two military powers could easily destroy each other and all others on the planet,” he noted.
“US policy in the Middle East has no clear vision. It claims it wants an end to ISIS yet seems to be dancing around when it comes to going after them. Are they waging a war against ISIS? Or, are they funding and supplying them? Or is the US goal foremost to take out the Assad government, with any damage to the ISIS powers being secondary?” the analyst wondered.
“It is not hard to believe that all that Turkey has been doing has been with full knowledge of its US controllers. Its primary goals are to see an end to the Assad regime (similar to that of the US) but also to prevent any kind of Kurdish independence,” he stated.
“Turkey knows that what it does militarily will be supported by NATO so all such actions must have US approval which would draw the Russian military into a combat situation with the US or its allies,” Hoenig concluded.
US 'concerned' over S-400 deployment
The Kremlin has announced that it is sending S-400 anti-aircraft missiles to Latakia in northwestern Syria in the wake of the shooting down the Russian warplane.
The US military is very concerned about Russia’s imminent deployment of the advanced missile defense system to Syria, according to an American official.
The official, speaking on condition of anonymity, said on Wednesday the S-400 poses a significant threat. He said the planned deployment is raising “significant concerns” for the US military, which is conducting airstrikes in Syria.
Game-Changing Treatment Restores Production of Insulin
Could this be the end of daily injections for people with Type 1 diabetes? 'Game-changing' treatment restores production of insulin
- Type 1 diabetes is a condition where the immune system attacks insulin-producing cells in the pancreas, stopping them producing the hormone
- Experts found injecting immune cells into the body protects the pancreas
- Treatment restored the production of insulin for a year and was safe
- Could end need for injections and prevent the disease from progressing
Published:
09:57 GMT, 26 November 2015
|
Updated:
10:29 GMT, 26 November 2015
Millions
of people with Type 1 diabetes may be freed from injecting themselves
with insulin every day after a breakthrough discovery.
Scientists
have found that injecting billions of immune cells into the body
restores the production of the hormone, which breaks down sugar in the
blood.
Experts said the treatment, which lasted for a year, could be a ‘game-changer’ for people with the disease.

+4
Millions of people with Type 1
diabetes may be freed from inject themselves with insulin every day,
scientists claim. They found injecting billions of immune cells into the
body restores the production of the hormone
Diabetes is a life-long health condition where there is too much glucose in the blood because the body cannot use it properly.
Insulin is the hormone secreted by cells in the pancreas which breaks down sugar in the blood.
Healthy
people have millions of ‘T-reg’ cells which stop the body’s immune
system attacking these insulin-producing cells in the pancreas.
However,
people with Type 1 diabetes do not have enough T-reg cells to protect
the pancreas, and so it is attacked and stops making enough insulin.
Everyone diagnosed with Type 1 is treated with insulin, and the majority inject themselves with insulin multiple times daily.
RELATED ARTICLES
Share
1.2k shares
Now,
Californian researchers have found that T-reg cells can be removed from
the body and increased by 1,500 times in a laboratory, the Telegraph reports.
Then, they can be put back into the bloodstream and will function normally to protect the insulin-producing cells.
A trial of 14 people found the treatment is safe - and lasts up to 12 months.
The people in the study were aged between 18 and 43 and had recently been diagnosed with Type 1 diabetes.
Doctors removed around two cups of blood containing two to four million T-reg cells.
These were separated from other cells and allowed to replicate in a laboratory, before being infused back into the blood.

+4
Insulin is the hormone secreted by
cells in the pancreas (pictured) which breaks down sugar in the blood.
People with type 1 diabetes stop making insulin as the body's immune
system attacks cells in the pancreas
A
quarter were found to be there after 12 months, and they were able to
protect the pancreas so it could continue to produce insulin.
Professor Jeffrey Bluestone, of the University of California San Francisco, told The Telegraph: ‘This could be a game-changer.
‘By using T-regs to “re-educate” the immune system, we may be able to really change the course of this disease.
This could be a game-changer
Professor Jeffrey Bluestone, of the University of California San Francisco
‘We expect T-regs to be an important part of diabetes therapy in the future.’
The therapy could stop the need from regular insulin injections.
It could also stop the disease from progressing, leading to organ damage, blindness and limb amputations.
The
team added that the treatment could be developed in future to help
people with other autoimmune diseases such as rheumatoid arthritis and
lupus.
It may even help people with cardiovascular disease, neurological disease and obesity.
The research was published in the journal Science Translational Medicine.
WHAT IS THE DIFFERENCE BETWEEN TYPE 1 AND TYPE 2 DIABETES?
Type 1 diabetes
Type
1 develops when the insulin-producing cells in the body have been
destroyed, leaving the body unable to produce any insulin at all.
Everyone diagnosed with Type 1 is treated with insulin.
Scientists don't know why the insulin-producing cells are destroyed in people with the condition.

+4
All those diagnosed with Type 1 diabetes are treated with insulin, pictured
It
is thought to be caused by an abnormal, autoimmune, reaction to the
cells, which could be triggered by a virus or other infection.
Experts believe there is a genetic element to Type 1 diabetes.
It is more common in some parts of the world than others.
Unlike Type 2, Type 1 diabetes has nothing to do with lifestyle or weight.
The condition can develop at any age, but is usually diagnosed before the age of 40, most commonly in late childhood.
Around 10 per cent of the 2.9 million people diagnosed with diabetes in the UK have Type 1.
Type 2 diabetes
The condition develops when the body is still able to make insulin, but not enough.
It also develops when the insulin that is produced by the body does not work properly - known as insulin resistance.
Initially, Type 2 diabetes can be controlled with a healthy diet and regular exercise.

+4
Being obese or overweight is the biggest risk factor for developing Type 2 diabetes
Medication is also often required and a large number of sufferers eventually progress to needing insulin.
People
who are overweight and have a large waist, are more likely to be
diagnosed with Type 2 diabetes - it is the biggest risk factor.
Those
who have a close relative with the condition, or who are from a black
or South Asian background are also at increased risk.
The condition usually affects those aged over 40, but people from South Asia are commonly affected from the age of 25.
Around 90 per cent of the 2.9 million people diagnosed with diabetes in the UK have Type 2.
Subscribe to:
Posts (Atom)


